Vol 10 | Issue 8 | August 2024 Indian J Case Reports 219
Case Report
Managing calcaneal fractures through modified sinus tarsi approach and headless screws fixation
Ahmed Samy Elhammady
Consultant, Department of Trauma and Orthopedic Surgery, Mallersdorf Hospital, Mallersdorf-Pfaffenberg, Germany,
ABSTRACT
The calcaneus is the most commonly fractured tarsal bone, and the treatment of patients with intraarticular calcaneal fractures remains controversial. Operative treatment utilizing extensile approaches provides excellent exposure of the fracture but is associated with high rates of wound complications. This case report discusses the application of the mini-open reduction technique through the modified sinus tarsi approach and fixation with headless cannulated screws for the reconstruction of an intra-articular tongue-type calcaneus fracture in a 67-year-old male patient who presented with a history of falling from a 2-meter height, sustained a dislocated intra-articular calcaneal fracture. Using a 2–3 cm lateral transverse incision, we reduced the fracture and percutaneously fixed it with two headless cannulated screws. The patient fully regained his activity level by the 3rd-month postoperatively. At the 9-month follow-up, foot and ankle functions were found to be satisfactory. Minimally invasive treatment of calcaneal fractures achieved through the modified sinus tarsi approach provides excellent fracture exposure and percutaneous fixation using headless cannulated screws ensures better outcomes.
Key words: Calcaneal fracture, Percutaneous screws, Intra-articular tongue-type fracture, Minimally invasive
Calcaneal fractures are one of the challenging injuries in orthopedic practice, which usually result from an axial compressive force, such as a road traffic accident or fall from height. Calcaneal fractures represent 1–2% of all human body fractures [1] and almost 60% of all tarsal fractures, and they are still a great challenge in terms of treatment [2,3]. Conservative treatment includes splinting, limb elevation, non-weight bearing for an average of 6 weeks, and then physiotherapy for rehabilitation which may take up to 2 years [4]. Several studies in the past have encouraged open reduction and internal fixation as the standard operative protocol, but there have been several complications associated with it [5].
This case report describes the repositioning of an intraarticular tongue-type calcaneus fracture through the minimally invasive modified sinus tarsi approach and fixation with headless cannulated screws.
CASE REPORT
A 67-year-old male patient was admitted to the emergency unit, presenting injuries sustained from a fall from a 2-meter-high ladder. The injury occurred 12 h ago.
The general physical examination revealed normal vital signs, and the ABCD assessment was within physiological parameters. Local clinical examination revealed limitations in movement, ecchymosis, and edema over both feet and ankles, along with a substantial blister on the left heel (Fig. 1). Tenderness and swelling were more pronounced on the left side. The neurovascular status was intact in both feet.
Anteroposterior, lateral (LAT), and oblique radiographs of both foot and ankle sides revealed a fragmented tongue-type calcaneus fracture on the left side (Fig. 2). A computer tomography scan of both ankle joints confirmed the displaced intra-articular tongue-type calcaneus fracture on the left side, with multiple fragments within the fracture cleft.
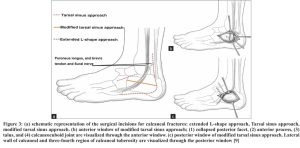
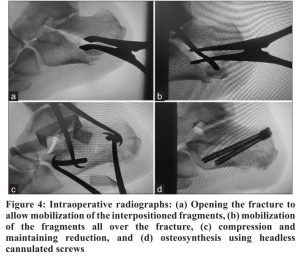
The patient underwent surgery on the 6th day following the traumatic incident. The procedure was performed under general anesthesia, with the patient positioned in full LAT decubitus, the left side facing upward, on a radiolucent operating table. Adequate padding was applied to support the right leg and prevent pressure on the peroneal nerve, and a tourniquet was not employed. First, the LAT malleolus, the base of the fifth metatarsal, and the path of the sural nerve were marked. A transverse incision was then performed 1.5 cm distal to the tip of the LAT malleolus along the calcaneal axis, extending from the base of the fourth metatarsal to 1 cm anterior to the Achilles tendon. This incision traversed over the sheath of the peroneus longus and brevis tendons, with careful attention paid to isolating and protecting the sural nerve during dissection. The operative field was delimited by the peroneus tendon sheath, defining the anterior and posterior windows of exposure (Fig. 3). By applying posterior traction to the peroneus tendon sheath, the anterior window was opened, providing visualization of structures including the anterior process, calcaneocuboid joint, and posterior facet. Partial division of the calcaneofibular ligament facilitated complete exposure of the posterior facet and any collapsed fracture fragments when necessary. The fracture line was utilized by employing a periosteal elevator from LAT to medial, facilitating the mobilization of fracture fragments. Following the removal of the comminuted fragments from the fracture cleft, two Steinmann pins were percutaneously inserted, both placed from LAT to medial. A reduction clamp was applied laterally over the pin, and another clamp was applied medially, ensuring optimal compression and maintaining reduction. It is noted that attempting repositioning with only one clamp on the LAT side would lead to LAT compression and medial distraction of the fracture. Following anatomic reduction, fixation was accomplished using two headless cannulated screws 7 mm. These screws were inserted from the posterior superior tuberosity, directed inferiorly and distally, (Fig. 4).
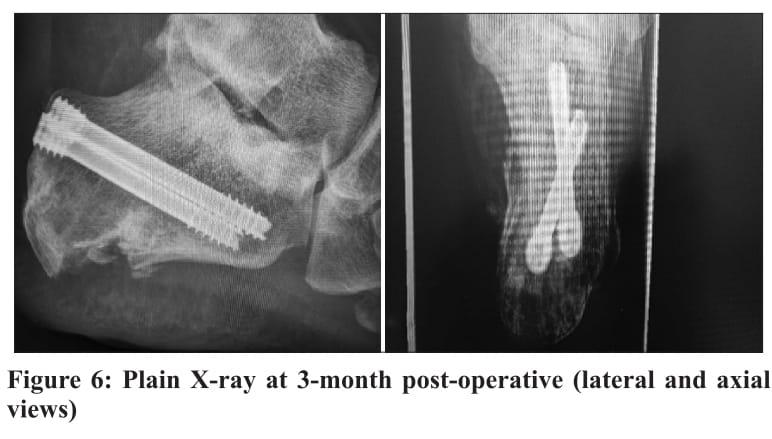
During the initial 2 weeks, the patient was wrapped in an elastic bandage and advised to engage in a gentle range of motion exercises for the ankle and subtalar joints. At the 2-week follow-up, with the wound fully healed, stitches were removed (Fig. 5). At 6 weeks, partial weight-bearing at 20 kg was initiated, utilizing an air cast walker, and a gradual progression to full weight-bearing was achieved by 10 weeks. X-rays were performed at 1-week, 6-week, 3-month, and 6-month postoperatively, (Fig. 6).

DISCUSSION
The optimal method for treating intra-articular fractures of the calcaneus remains controversial. Recent trends toward internal fixation have emerged in the past 5–10 years. This is in part attributable to the positive reports of surgeons with extensive experience treating calcaneal fractures. However, others question the extended LAT L-shaped approach has been widely used for plate fixation of calcaneal fractures and 60–85% of cases showed satisfactory clinical outcomes; however, it is accompanied by a high risk of soft tissue complications [8]. In a retrospective review of 112 operatively treated intra-articular calcaneal fractures, Klein et al. reported that the extensile approach group exhibited an overall wound complication rate of 29%, with 9% requiring operative intervention. In contrast, the minimally invasive approach group demonstrated a lower wound complication rate at 6%, with none requiring operative intervention (p=0.005) [7].
According to the previous reports, the subcutaneous tissues of the LAT hindfoot receive blood supply from two distinct systems: The upper flap is nourished by the LAT calcaneal artery and the LAT malleolar artery, while the tissue on the tarsal side is supplied by the LAT tarsal artery. Notably, the LAT calcaneal artery is situated proximal to the vertical portion of the conventional L-shaped incision, making it susceptible to injury if the incision is inaccurately placed. Moreover, the horizontal component of the traditional L-shaped incision poses a risk of damaging the vascular network supplying the plantar flap. Thus, occlusion or iatrogenic injury to the LAT calcaneal artery can lead to compromised blood supply to the LAT flap, resulting in vascular network disruption and complications in soft tissue healing [9].
In this study, the modified sinus tarsi approach prioritizes the preservation of the intricate LAT hindfoot anatomy and blood supply. By doing so, we effectively minimized the potential damage to the plantar blood vessels and safeguarded the integrity of the LAT calcaneal artery during surgical procedures. This modification significantly enhances the assurance of sufficient blood supply to the LAT flap, thereby optimizing surgical outcomes. In their study involving 29 patients, Zhan et al. concluded that, compared to the sinus tarsi approach, the modified sinus tarsi approach achieved wider exposure and provided rigid fixation for Sander’s Type II and III calcaneal fractures, thereby limiting soft-tissue complications [9].
The choice of osteosynthesis material is crucial in achieving a satisfactory result. One reported complication associated with the use of cannulated screws is skin and Achilles tendon irritation. In a study involving 33 patients, Abdelazeem et al. found that seven patients experienced tenderness at the posterior incision due to prominent screw heads at 3-month post-surgery and were managed by removal of the screws at 6 months after surgery [10]. In contrast, our study utilized thick headless screws that did not protrude through the skin, providing stable fixation without causing irritation to the skin or Achilles tendon.
In this case report, the mitigation of potential complications associated with the treatment of intraarticular tongue-type calcaneus fractures was achieved through four key measures. First: Soft-tissue issues were minimized by employing a 2–3 cm transverse incision in the posterior aspect of the modified sinus tarsi approach, ensuring excellent visualization of the fracture and the LAT wall of the calcaneus. Second: Optimal fracture reduction was achieved with percutaneous Steinmann pins, ensuring effective compression through indirect reduction using clamps the use of these operative techniques because of the possibility of catastrophic complications of open treatment. This especially is true in patients who are prone to infection from systemic illness, such as diabetes or from smoking [6,7].
The surgical treatment effects of calcaneal fracture vary with the surgical approach and operative methods and the incision complications directly affected the clinical results. Previously, placed over the pins, both medially and laterally, rather than solely on the LAT plane. This avoids also direct clamping over the calcaneus, preventing the risk of fragmentation, particularly in osteoporotic patients. Third: Applying cannulated screws with an appropriate thickness of 7 mm to prevent implant failure, particularly in cases of minimal thickness screws. Fourth: Opting for headless screws instead of headed screws to avoid tenderness and skin irritation caused by prominent screw heads.


CONCLUSION
This case report highlights the successful outcome of minimally invasive reduction for intraarticular tongue-type calcaneal fractures using the modified sinus tarsi approach which provided excellent exposure of the fracture associated with percutaneous fixation with 7 mm headless cannulated screws, contributing to the overall positive results.
REFERENCES